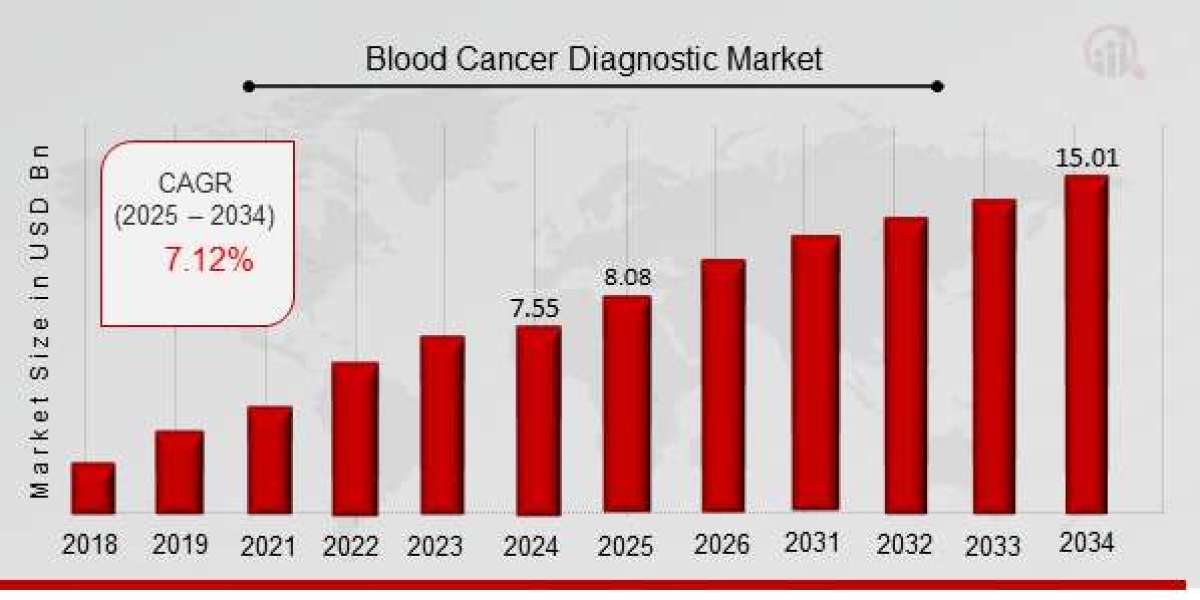
How Advances in Blood Cancer Diagnostics are Revolutionizing Early Detection in 2025
Blood cancers, which include leukemia, lymphoma, and myeloma, are among the most difficult to diagnose and treat due to their complex nature. Traditional diagnostic methods, such as bone marrow biopsies, blood tests, and imaging scans, have provided essential insights into the presence of these cancers. However, as the demand for more accurate, faster, and less invasive diagnostic techniques grows, advances in blood cancer diagnostics are making a significant impact in the field.
In 2025, these advancements are revolutionizing early detection, giving patients a better chance at successful treatment outcomes. This blog will explore how emerging technologies are transforming the diagnosis of blood cancers and why early detection is so crucial in improving survival rates.
The Need for Early Detection in Blood Cancer
Blood cancers, including leukemia, lymphoma, and myeloma, are often diagnosed at advanced stages when symptoms are more pronounced. However, early detection significantly improves a patient’s chances of survival and successful treatment. The challenge lies in detecting these cancers in their earliest stages when symptoms may be subtle or even non-existent. Early detection not only allows for timely interventions, but it also provides opportunities for more targeted therapies, which can result in better outcomes and a higher quality of life for patients.
Unfortunately, current methods for detecting blood cancer—like standard blood tests or invasive procedures—often fall short in identifying cancers at their earliest and most treatable stages. As a result, there has been a significant push within the medical community to improve diagnostic tools for blood cancer and catch these diseases before they progress.
Recent Advances in Blood Cancer Diagnostics
The field of blood cancer diagnostics has seen several breakthroughs over the past few years. The integration of cutting-edge technologies has significantly improved the accuracy, speed, and efficiency of blood cancer diagnoses. Here are some of the key advancements in the market:
1. Liquid Biopsy: A Non-Invasive Approach
One of the most promising advancements in blood cancer diagnostics is the use of liquid biopsy, a minimally invasive technique that analyzes blood samples to detect genetic mutations, tumor markers, and abnormal cell populations that indicate the presence of cancer. Liquid biopsies are capable of detecting circulating tumor DNA (ctDNA), RNA, and other biomarkers that provide insights into the presence and progression of blood cancers.
Unlike traditional biopsies, which require tissue samples from bone marrow or lymph nodes, liquid biopsies can be performed using only a blood draw, making them less invasive and quicker to process. Liquid biopsy also allows doctors to monitor treatment progress and detect minimal residual disease (MRD)—tiny amounts of cancerous cells that may remain after treatment and could cause a relapse. This capability helps guide decisions on whether additional treatment is necessary, making it an invaluable tool in early detection and ongoing monitoring.
In 2025, liquid biopsy technology continues to advance, offering even more sensitive and specific testing methods for various blood cancers. For example, studies are showing its potential for detecting early-stage leukemia and lymphoma, which were traditionally difficult to diagnose at an early stage.
2. Artificial Intelligence (AI) and Machine Learning
The use of artificial intelligence (AI) and machine learning in blood cancer diagnostics is a game-changer. AI algorithms are now being applied to large datasets, such as blood tests and imaging scans, to help identify patterns and biomarkers associated with blood cancers. These technologies can process vast amounts of information much faster and more accurately than human clinicians, enabling earlier identification of cancerous changes in the blood or bone marrow.
AI models can also assist pathologists in analyzing digital slides and detecting abnormalities that may otherwise go unnoticed. This reduces diagnostic errors and ensures more accurate diagnoses, leading to timely treatment and better patient outcomes. AI-powered diagnostic tools are also being integrated into liquid biopsy systems, further enhancing their sensitivity and specificity.
One of the most promising aspects of AI in blood cancer diagnosis is its ability to identify rare genetic mutations or unique subtypes of blood cancers that traditional methods may miss. By continuously learning from new data, AI systems will only improve their diagnostic capabilities, making early detection faster, more accurate, and more accessible.
3. Genomic and Molecular Diagnostics
The use of genomic testing and molecular diagnostics is also improving the precision of blood cancer diagnoses. Genomic testing involves sequencing the genetic material from a patient’s blood or tissue sample to identify mutations or genetic alterations that could be causing the cancer. By pinpointing the specific genetic drivers of the disease, doctors can better understand the nature of the cancer and tailor treatments accordingly.
For instance, certain genetic mutations, such as BCR-ABL1 in chronic myelogenous leukemia (CML), are associated with targeted therapies that can significantly improve treatment outcomes. Genomic and molecular tests can identify these mutations early, guiding doctors in prescribing the most appropriate treatment.
In addition to sequencing technologies, next-generation sequencing (NGS) is gaining traction in the field of blood cancer diagnostics. NGS is a highly sensitive and accurate method for detecting mutations and chromosomal abnormalities, allowing for a more comprehensive view of the disease. It can also be used to identify minimal residual disease, offering doctors a powerful tool for monitoring patients in remission.
The Role of Early Detection in Improving Treatment Outcomes
Early detection of blood cancer has a significant impact on treatment success. When diagnosed early, blood cancers are generally more responsive to treatments, and the likelihood of remission increases. Early-stage blood cancers often require less aggressive treatment and are less likely to spread to other organs, improving the patient’s prognosis.
Moreover, early detection allows for better personalized medicine—treating patients based on their genetic profile and specific tumor characteristics. The growing availability of targeted therapies—medications designed to specifically target the molecular drivers of cancer—means that early detection is key to identifying which treatments will be most effective.
For example, in cases of chronic lymphocytic leukemia (CLL), early identification of mutations can guide the use of targeted therapies, such as BTK inhibitors, which specifically target the abnormal cells that cause CLL, offering more effective and less toxic treatment options.
Conclusion
The advances in blood cancer diagnostics are making early detection more achievable than ever before. Technologies such as liquid biopsy, artificial intelligence, and genomic testing are enabling clinicians to detect blood cancers earlier, monitor disease progression, and offer more personalized and targeted treatments. As these innovations continue to evolve, they will undoubtedly improve the survival rates and quality of life for patients diagnosed with blood cancers.
In 2025, the future of blood cancer diagnostics looks promising, with continuous improvements in accuracy, accessibility, and non-invasive techniques. Early detection remains the key to unlocking better treatment outcomes, and these breakthroughs are pushing the boundaries of what’s possible in the fight against blood cancers. The next few years hold great promise for advancements in diagnostic capabilities, offering hope to millions of people worldwide.